Have questions? Contact the Benefits Service Center at 704-631-1500, Option 1, 7:30 a.m. to 8:00 p.m., Monday-Friday.
We have been made aware that a recent provider-based marketing email titled “Open Enrollment is now open” was sent to Atrium Health patients on Nov. 7. The communication is not related to our teammate Annual Enrollment period, which was Oct. 23 through Nov. 3. This email is about the Health Insurance Marketplace’s Open Enrollment period. To review your 2024 Annual Enrollment benefit elections in CORE Connect, navigate to Me > Benefits > Your Benefits. Select Open Enrollment from the drop down and select View Benefits Summary in the top right corner.
Post-Annual Enrollment Checklist
Print your confirmation statement.
- Always keep a copy of your confirmation statement in a safe location.
- In the event of any coverage discrepancies, you will be asked to provide a copy of your confirmation statement as proof of enrollment.
- Navigate to Me > Benefits > Your Benefits.
- See Benefits as of Date or Event: Select Open Enrollment
- View Benefits Summary in the upper right corner of the screen.
Have questions about your submitted Annual Enrollment elections?
- Call the Benefits Service Center at 704-631-1500, Option 1, 7:30 a.m. to 8:00 p.m. Monday - Friday, immediately for assistance.
Are you a New Hire?
- Submit your new hire elections as soon as possible.
- Once you have submitted, please call the Benefits Service Center at 704-631-1500, Option 1, 7:30 a.m. to 8:00 p.m. Monday - Friday.
- The Benefits Service Center will trigger your Annual Enrollment event for you, allowing you to elect your 2024 benefits.
Experiencing a Life Status Change (LSC)?
- If you experience a Life Status Change between now and the end of the year, contact the Benefits Service Center at 704-631-1500, Option 1, 7:30 a.m. to 8:00 p.m. Monday - Friday, for assistance.
- The Benefits Service Center will trigger your LSC for you.
- Once you have submitted your LSC elections, please call the Benefits Service Center back so that they can trigger your Annual Enrollment event, allowing you to elect your 2024 benefits.
If you have had trouble accessing CORE Connect to enroll, please note the following:
- If you are trying to access from a shared computer, be sure to login to Webapps first, and then login to CORE Connect from your Webapps.
- If you are timed out of CORE Connect while enrolling, close your browser window and access CORE Connect again from PeopleConnect on an individual computer, or Webapps on a shared computer.
- If you see the Oracle Applications Cloud sign in screen, click Company Single Sign-On. Do not enter your User ID and Password.
Jump to:
2024 Annual Enrollment Resources
2024 Annual Enrollment Highlights
- Health Plan Updates:
- Health Savings Plan
- Deductibles are increasing to $1,600 for teammate-only coverage and $3,200 for family coverage
- Co-Pay Plan
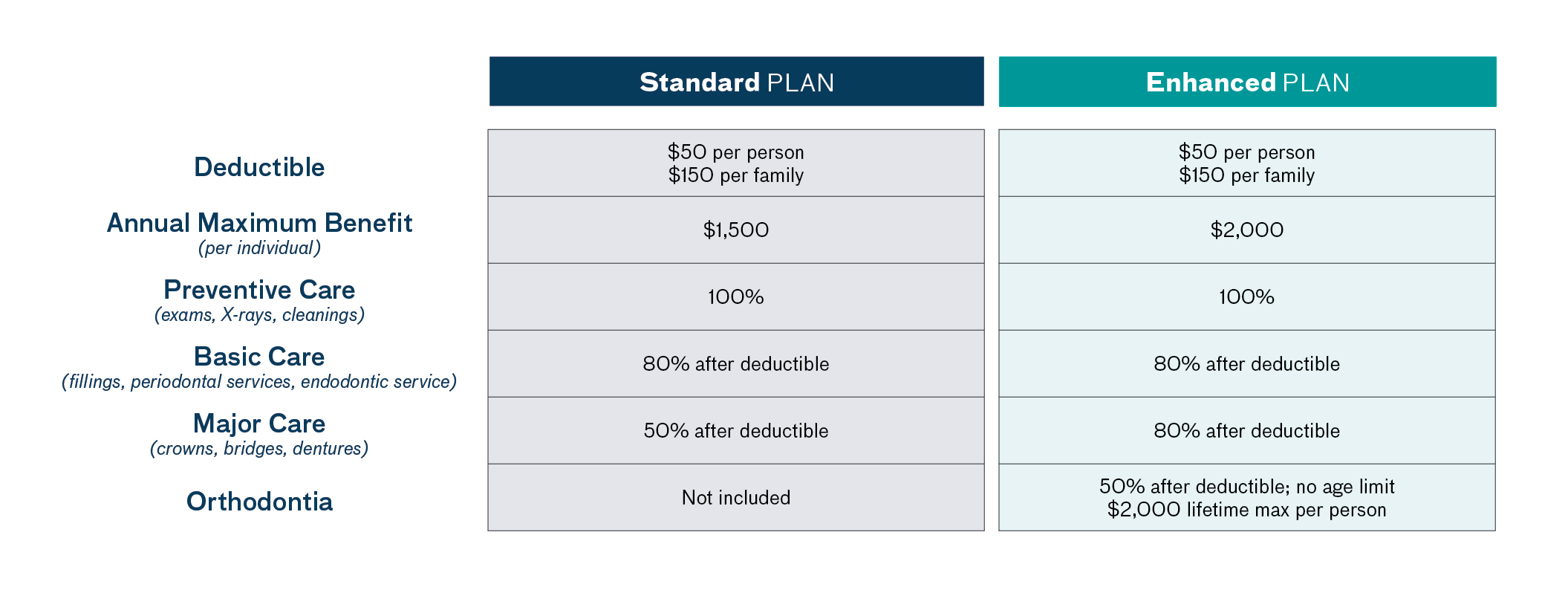
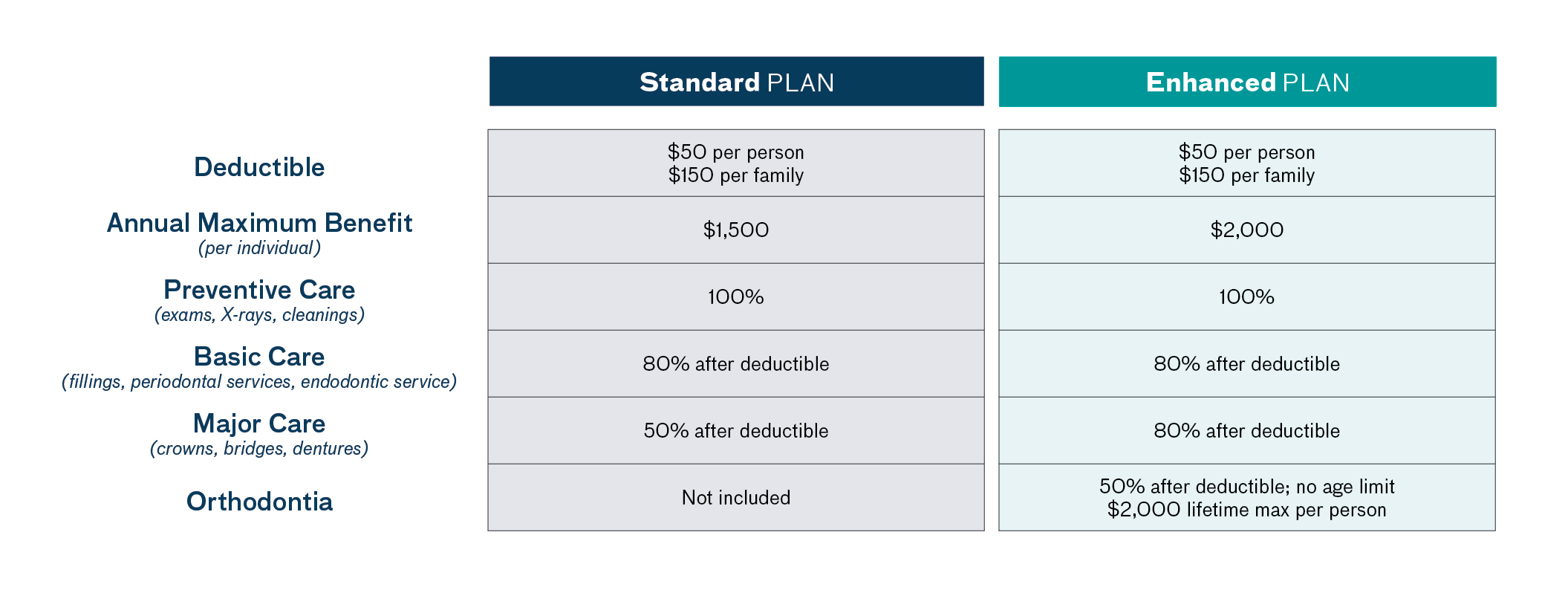
- Second Dental Plan with Delta Dental added to provide choice:
- Both plans offer 100% coverage for preventive care and 80% coverage for basic care
- Both plans provide you with comprehensive coverage at the provider of your choice
- IMPORTANT NOTE: Teammates currently enrolled in the 2023 Dental Plan and who do not complete a Dental election during Annual Enrollment, will have their Dental enrollment for 2024 defaulted to the Standard Plan at the same coverage tier.
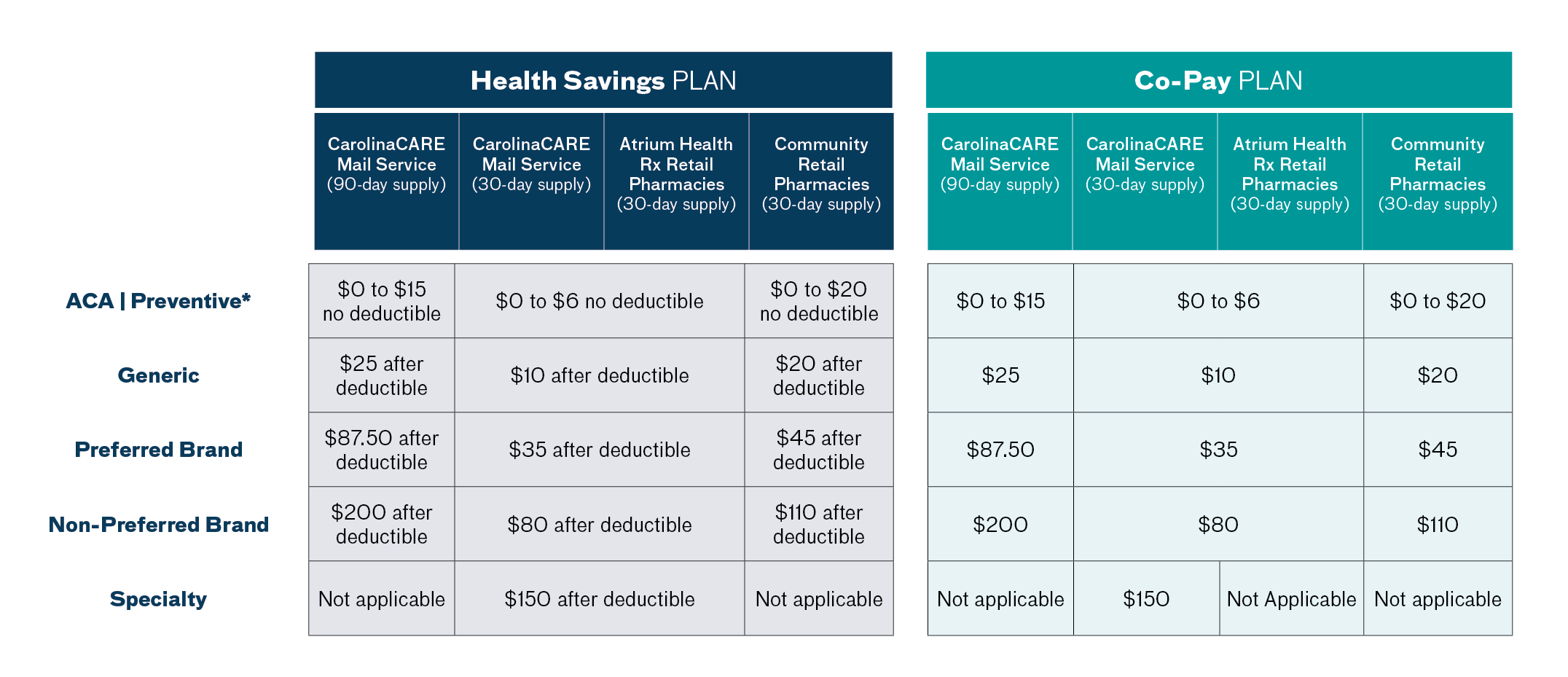
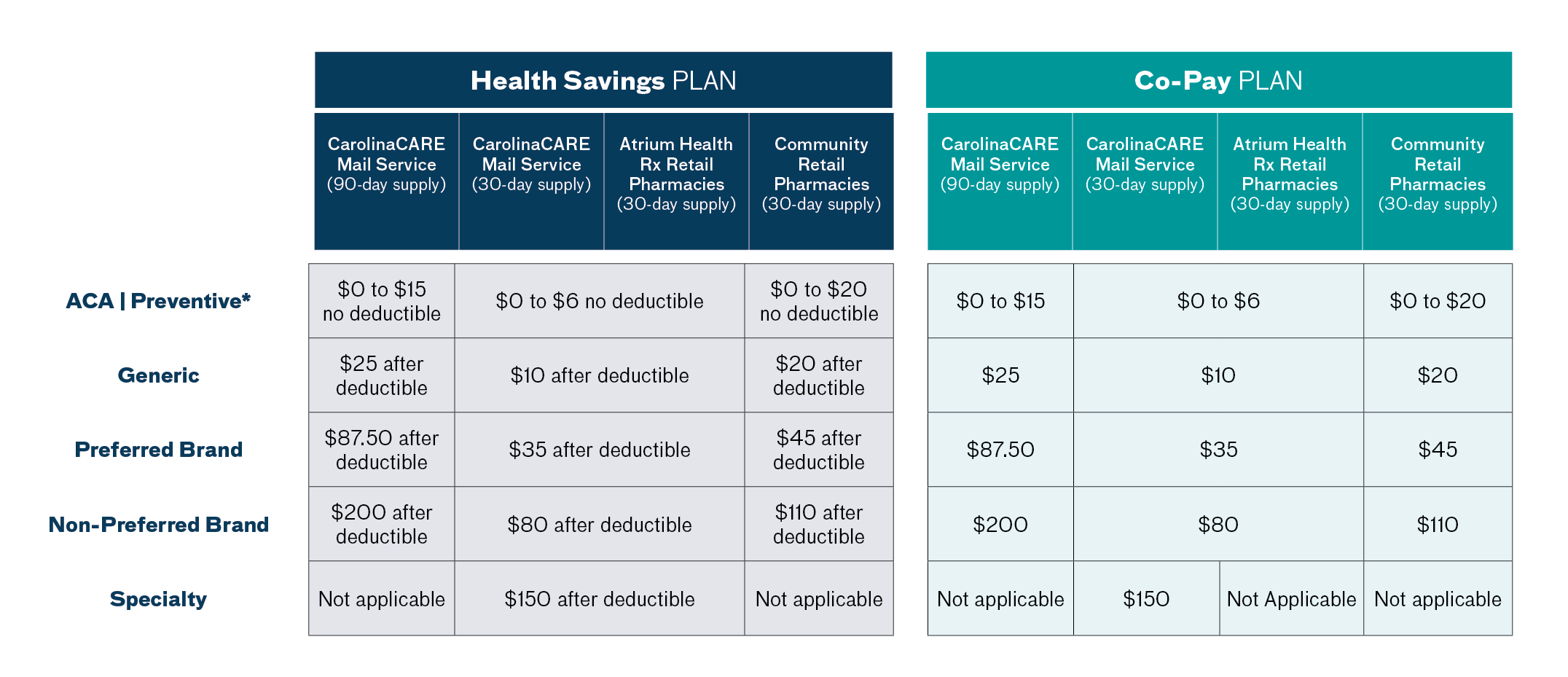
- CarolinaCARE is growing and implementing best in class software to most effectively serve teammates and health plan members. In 2024, the new platform will no longer have a payroll deduction option. Teammates can use their HSA or FSA cards as their primary form of payment for a tax-free way to pay for prescriptions. Most major credit cards and debit cards can also be used to pay for prescriptions. Plan to update your payment method, if applicable. Here is what you need to know in order to be ready for the change on Jan.1, 2024.
- Why is payroll deduction going away? CarolinaCARE is growing and implementing best in class software to serve teammates and health plan members most effectively. In 2024, the new platform will no longer have a payroll deduction option.
- What other options can I use to pay for my prescription orders at CarolinaCARE? As of Jan. 1, 2024, you can pay for prescription orders using your Health Savings Account (HSA) card, Flexible Spending Account (FSA) card, credit and debit cards such as Visa, Mastercard, American Express and Discover.
- Is there an advantage to using my HSA or FSA card instead of a regular credit or debit card? Yes. Teammates can use their HSA or FSA cards for a tax-free way to pay for prescriptions and other qualified medical expenses.
- I currently use payroll deduction as a back-up to my HSA or FSA card whenever all my funds are spent. What will happen when payroll deduction goes away? Again, when payroll deduction is no longer available as of January 1, 2024, you will be able to use your HSA or FSA account cards, credit and debit cards to pay for prescription orders.
- What steps can I take during the 2024 health benefits Annual Enrollment period (Wednesday, Oct. 18, through Friday, Nov. 3) to plan for the removal of payroll deduction to pay for prescriptions? It is important to review the cost of all medications and medical supplies that you and your family currently use. Try to anticipate any other prescription needs you may have in 2024 (to include over-the-counter medications like vitamins, cough and cold products, and allergy relief). The CarolinaCARE prescription price estimator may be a helpful tool to guide you in adding up the expenses. This way, you can make a better estimate of the amount that you will need to contribute to your HSA or FSA account to cover costs for the entire year.
- During the Annual Enrollment period for 2024 benefits (Wednesday, Oct. 18 through Friday, Nov. 3), you may want to make an online appointment and speak with a pharmacist at One-on-One Rx about your medicine costs. Visit www.CarolinaCARERx.org for more information about how to schedule an appointment.
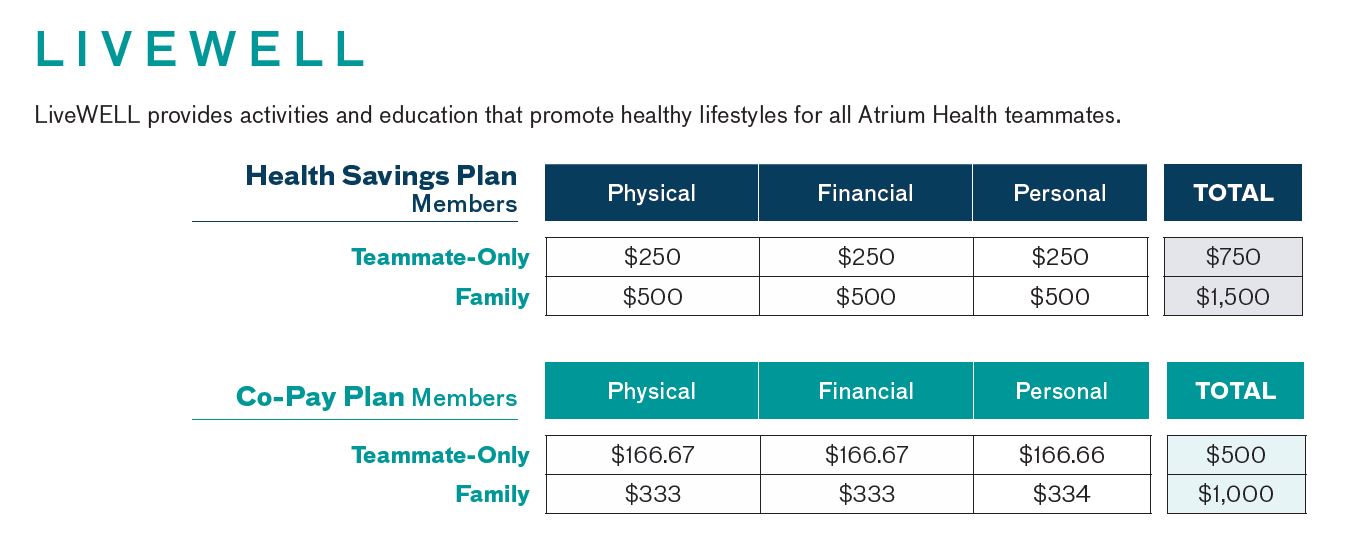
- LiveWELL incentives are changing
- For teammates enrolled in the Health Savings Plan, you can earn $750 in incentives for teammate-only coverage and $1,500 for family coverage.
- For teammates enrolled in the Co-Pay Plan, you can earn $500 in incentives for teammate-only coverage and $1,000 for family coverage.
Completing Your Enrollment
In CORE Connect, navigate to:
- Me
- Benefits
- Make Changes (under your name in the center of the screen)
- You will be prompted to review your dependents
- Select ‘+Add’ next to People to Cover to add any new benefits eligible dependents that aren’t appearing on the screen
- You do not need to add the same dependent more than once
- If the dependent listed on the screen is benefits eligible, you will be able to elect coverage for that dependent in your Annual Enrollment event
- If you need to modify an existing Dependent:
- Select their name on the screen
- Select the pencil next to the section that you want to modify
- After modifying the information select Submit
- Note: If you are correcting data on the dependent’s record, for example their name, change the effective date of the edit to match the relationship start date of the dependent
- Select the back button next to the dependent’s name
- Select Continue
- Review and accept the Attestation
- Make your 2024 Annual Enrollment changes by selecting the pencil next to each benefit category
- Click Continue to review your elections; edit as necessary
- Submit your elections!
- Review and save a copy of your confirmation statement
- Navigate to Me > Benefits > Your Benefits
- Select Open Enrollment from the dropdown box and select View Benefits Summary in the upper right corner
If you have had trouble accessing CORE Connect to enroll, please note the following:
- If you are trying to access from a shared computer, be sure to login to Webapps first, and then login to CORE Connect from your Webapps.
- If you are timed out of CORE Connect while enrolling, close your browser window and access CORE Connect again from PeopleConnect on an individual computer, or Webapps on a shared computer.
After Enrollment: To print or save a copy of your Benefits Confirmation Summary
In CORE Connect:
- Click the Benefits tile.
- Then click the Your Benefits tile.
- On the Select a Benefit screen:
- Ensure the See Benefits as of Date or Event drop-down menu has Open Enrollment selected.
- In the top right corner of the page, click the View Benefits Summary button.
- A PDF file opens. Review the information in the PDF for accuracy.
- Save a copy of the PDF to your computer or print a copy for your reference later.
Summaries of Benefits and Coverage (SBCs)
Access your 2024 SBC by selecting your benefit plan below.
Important Reminders
- You must enroll in Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) each year. These elections do not carry over to the next benefit plan year.
- Add any new dependents before you start your enrollment.
- Ensure that dependent birthdates and Social Security numbers are correct.
- If you are enrolling a dependent child who does not live with you, be sure that you have their home address updated in their dependent record.
- View the steps on how to complete your enrollment.
Evidence of Insurability (EOI) Rules
Some changes to your existing life insurance elections may require EOI. If your election is subject to EOI, you must complete the EOI process and be approved by MetLife before new or increased coverage can take effect.
| Benefit |
EOI is Required For: |
EOI is Not Required For |
| Supplemental Teammate Life and AD&D |
- Any teammate who elects to increase the amount of their coverage by more than one level above their current amount of coverage
|
- Any teammate who elects to increase the amount of their coverage by only one level above their current amount of coverage
|
| Supplemental Spouse Life |
- Elections that are greater than $50,000
- Elections that are more than one level above the current amount of coverage, up to $50,000
|
- Elections to increase the current amount of coverage by one level, up to $50,000.
|
Short Term Disability (STD)
|
- Adding STD coverage for the first time during Annual Enrollment
|
- Increasing your existing voluntary STD coverage for the upcoming benefits plan year, from the 30-day option to the 14-day option
|
Voluntary Benefits
Voluntary benefits offerings for 2024 will be the same as what was offered for 2023. Review our Voluntary Benefits page for details on our voluntary benefit offerings.
Prescription Coverage
Please see below for prescription coverage as well as links to the CarolinaCARE Rx website and various prescription lists.
Resources
LiveWELL Incentives FAQs
Teammates have the opportunity to earn LiveWELL Incentives based on engagement in healthy lifestyle activities. Incentive opportunities vary by plan.
What are LiveWELL Incentives?
In 2024, teammates will have the opportunity to earn LiveWELL Incentives based on engagement in healthy lifestyle activities.
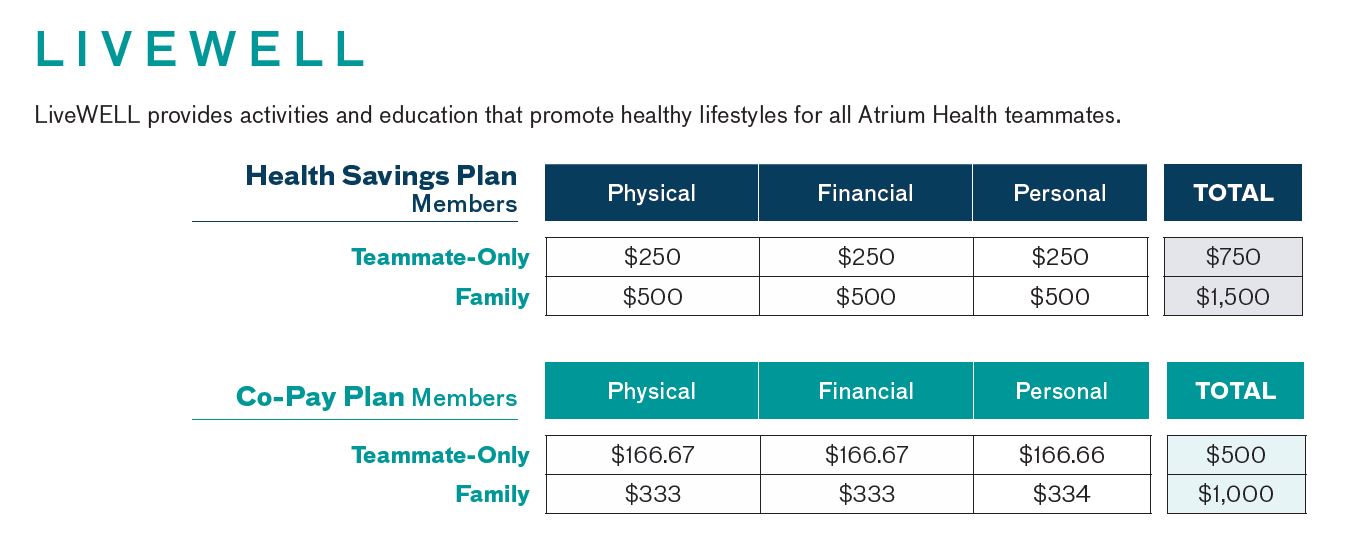
Is there an Incentive earned for completing the Health Assessment?
There is not a separate incentive earned, but the first step to begin the LiveWELL experience is completing the health assessment.
If I have a change in coverage from Individual to Family or from Family to Individual in the middle of the year, will the incentives I’ve earned and received payment for be adjusted accordingly?
Incentives earned and paid prior to a change in coverage will not be adjusted up or down for the new coverage tier. Any incentives earned after the coverage change will be paid at the current coverage level.
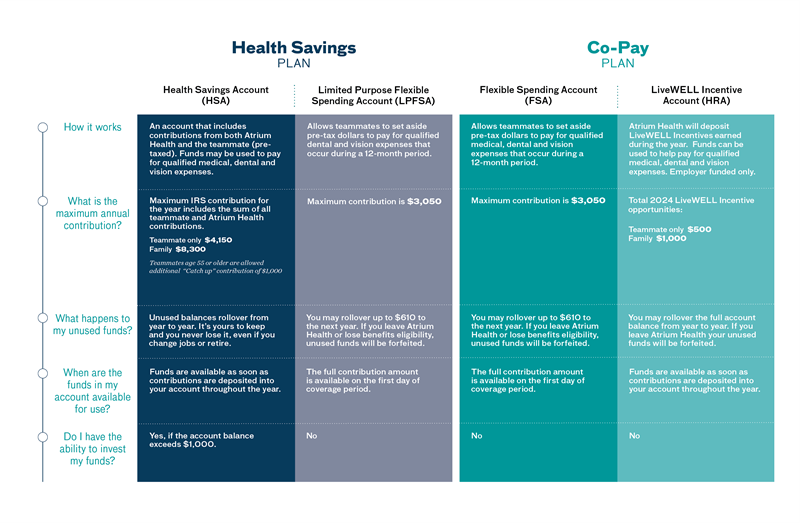
If I am enrolled in the Health Savings Plan, where will my earned LiveWELL Incentives be deposited?
Your earned LiveWELL Incentives will be deposited into your Health Savings Account (HSA) if you have an active HSA contributing at least $1 per pay period.
If you are enrolled in the Health Savings Plan without an active HSA, your LiveWELL Incentives will be paid as taxable earnings in your paycheck. Reasons for not having an active HSA may include the fact that you are enrolled in Medicare or TRICARE.
If I am enrolled in the Co-Pay Plan, where will my earned LiveWELL Incentives be deposited?
Your earned LiveWELL Incentives will be paid into your LiveWELL Incentive Account. If you do not have an active LiveWELL Incentive Account at the time of incentive payout, one will be opened for you.
Vision Coverage
Vision benefits offerings for 2024 will be the same plan design as what was offered for 2023. There will be a slight premium increase in 2024 shown below. To learn more about Community Eye Care (CEC) vision benefits click here.
| Coverage |
Full-Time* |
Part-Time* |
| Teammate-only |
$6.14 |
$6.14 |
| Teammate + One Dependent |
$11.83 |
$11.83 |
| Teammate + Family |
$17.72 |
$17.72 |
Deducted 26 times per calendar year (Note: Monthly teammates multiply premium by 26 and divide by 12.)
*Full-time premiums apply to teammates with standard hours of 30 or more per week (60 or more per pay period.)
**Part-time premiums apply to teammates with standard hours of 16-29 per week (32-59 per pay period.)
Saving and Spending Accounts
In 2024, the following IRS annual maximum limits for Savings and Spending Accounts will apply:
- Health Savings Account (HSA): $4,150 for teammate-only coverage and $8,300 for family coverage
- The maximum IRS contribution for the year includes the sum of all teammate and employer contributions, including incentives
- Teammates age 55 or older are allowed an additional “catch-up” contribution of $1,000
- Healthcare Flexible Spending Accounts (FSA): $3,050
- Limited Purpose Flexible Spending Accounts (LPFSA): $3,050
- Dependent Care Flexible Spending Accounts (DCFSA): $5,000 (no change from 2023)
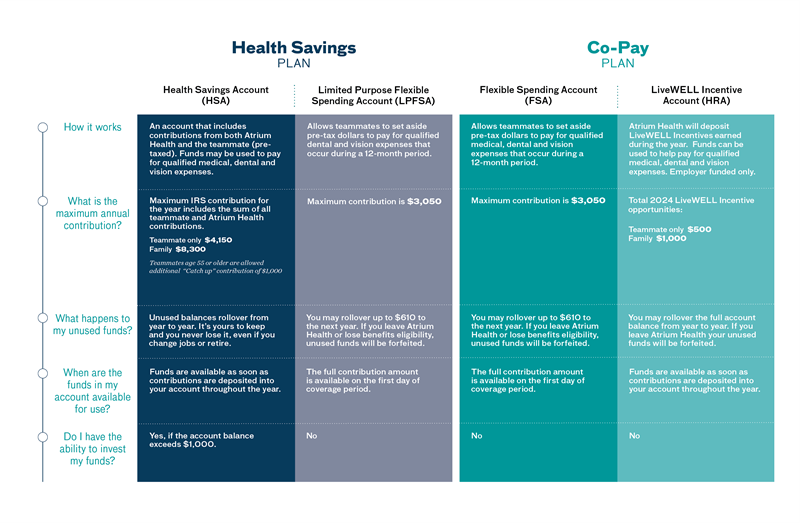
If you have questions regarding your accounts, please call Bank of America directly at 866-791-0250 or visit myhealth.bankofamerica.com.
Have Questions?
Contact the Benefits Service Center at 704-631-1500, Option 1, 7:30 a.m. to 8 p.m., Monday-Friday.